09. Inflamed Mind: Focusing on novel neuroinflammatory biomarkers and targets in understanding and managing suicide
Inflamed Mind: Focusing on novel neuroinflammatory biomarkers and targets in understanding and managing suicide
Prof. Xenia Gonda, MA (Psychology), PhD (Psychiatry), PharmD, Hungary
Department of Psychiatry and Psychotherapy, Semmelweis University New Antidepressant Target Group & MTA-SE Neurochemistry and Neuropsychopharmacology Research group, Semmelweis University and Hungarian Academy of Sciences
Laboratory of Suicide Prevention and Research, National Institute for Psychiatry and Addictology
Inflamed Mind: Focusing on novel neuroinflammatory biomarkers and targets in understanding and managing suicide
Abstract:
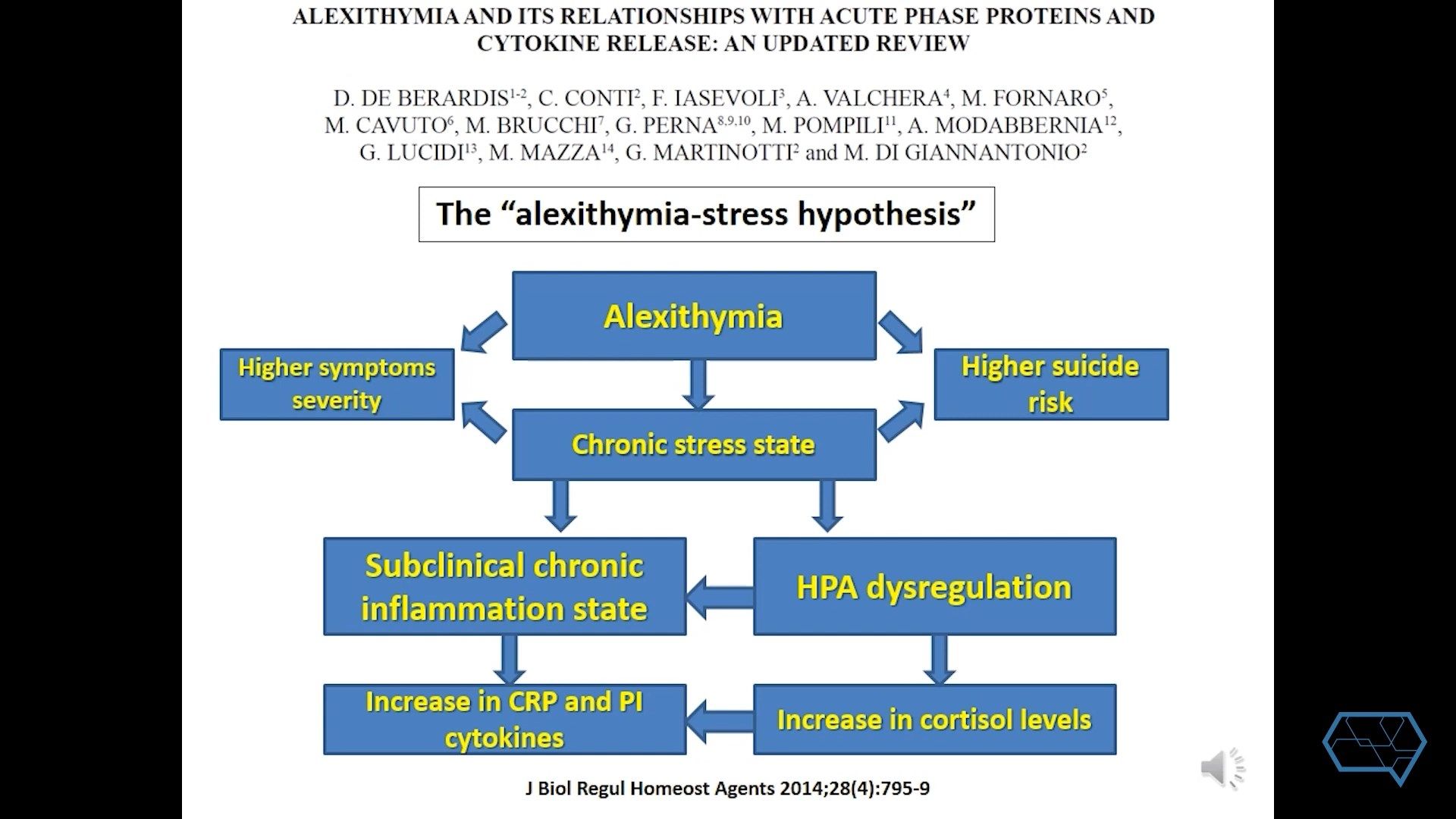
Suicide has a huge impact not only on the lives of patients and their families but also mental healthcare, public health and the society in general. In spite of these, we face several unmet needs in understanding, prevention and management of suicide. Our current methods of screening and predicting are highly unspecific and have a low predictive value, thus novel approaches to the etiology of suicide are needed to develop reliable biomarkers. An increased inflammatory state is present in suicidal patients with elevated levels of proinflammatory cytokines and a typical inflammatory signature profile. Based on understanding these processes we have the hope of repurposing currently used antiinflammatory molecules and developing novel ones which specifically target neuroinflammatory components of suicide.